Is this blog for adults or for kids?
Yes.
Snack Time. But first…
I’m going to start writing this article, but first I need a snack.
And if I go get a snack, I might see that there is a little bit of laundry that needs to be done. And just a few dishes.
But then I’ll remember the grilled cheese in the pan because of the burning smell.
Oh! I need to write!
Wait–but I’m still hungry. I remember making a grilled cheese…
I’m putting my blinders on so I can go retrieve a snack and get right back to you. I have important information about appetite and… the cacti are in bloom right now, but the blooms are fading and I noticed that at higher elevations they are still in bloom. Maybe I need to drive to Sedona. I could dictate this article on the drive.
Why am I hungry again?
Attention Deficit Hyperactivity Disorder.
I wasn’t diagnosed as a child. My symptoms were very subtle. I had no attention span and I had bursts of extreme energy. Subtle. Because of this, [insert dance party break].
Whatever. I think I was about to shift to discussing meds. I never had meds–Oh right, that’s where I was. I was left to cope and learn how to mask. I stim in my mouth and with my hands and with my eyes, a throwback to the more full-body movements I was told to stop doing “Because people will think there is something wrong with you.” I can still hear it in my head–you too? Jeez.
Medications and Appetite
Kids these days have all the meds. There are pros and cons, but I’m going to leave that discussion and decision up to you and the medical providers who are assessing growth, development, and symptoms. You know, the ones familiar with your family’s medical history and who have some understanding of your family’s dynamics and needs before offering advice. You see? I can’t do that in a blog. I can’t ask you questions, so I also can’t adjust the standard advice to fit your family comfortably.
Neurodivergence often comes along with food-related obstacles that require a shift in how we approach food. This is a great article on RDs for Neurodiversity that really gets into that aspect. In short, those with ADHD have the double-edged sword of distraction and hyperfocus. It may be more difficult to pay attention to cues and stop to take care of themselves. At the same time, it can be challenging to focus on putting together the meal.
Back to meds. The pharmaceutical treatments for ADHD often impact appetite. It’s common to get a call from a parent concerned about their child’s low weight, drive to sweets, and often insomnia to boot. Childhood is also a time of rapid brain development. The results of inadequate nutrition during this time can be detrimental and long-term.
At the same time, it’s essential to allow children to have the most freedom and independence it’s safe to provide. At the table, this means backing off– creating a dynamic that allows the child to serve themselves, determine whether and how much to eat, and account for their sensory and experience needs with foods served and with the environment. Yeah, this is where some one-on-one help can really… umm … help.
There is such a pretty butterfly on my yellow bell plant.
(editor note: take this out. It’s irrelevant.
writer response: no, it was pretty)
This article ADHD and Eating Habits provides this wisdom before going into more detail about ADHD and eating disorders:
ADHD symptoms and medications may make children, in particular, more vulnerable to
- undereating during the day
- overeating in one sitting
- and developing specific food fixations
When someone gets to the point of being overly hungry, they may find themselves craving and reaching for convenient, high-calorie, and quickly satisfying foods.

Certain psychostimulant medications are associated with a decrease in appetite. Somehow there is an inverse relationship here that results in these kids actually being a higher weight than expected. The interplay between diet, ADHD, and body weight is complex. So, as always, I’ll focus on the predictable and the possible. Not the scale.
It’s reported that up to 60% of children experience reduced appetite on medications. The most common being Methylphenidate products (Concerta, Ritalin, Focalin, etc) and amphetamine products (Adderall, Vyvanse, etc) Up to 15% of children experience no appetite at all (Strattera, Intuniv).
Another 40% of kids report abdominal pain, and 20% report headaches. All of these come into play where weight, appetite, and eating habits are concerned.
Some Practical Tips
Regis, I’d like to Phone A Friend!
(this is a reference to Who Wants to be a Millionaire, obvs)
Diana Rice, RD, friend, colleague, and fellow ADHD-er, owner of Tiny Seed Family Nutrition and the voice behind @anti.diet.kids (I know–she is so awesome) gives a few really practical tips:
- The main thing: Parents have to be pretty intentional about serving a sizable, palatable meal pre-meds and after they wear off.
- You may have to reconsider your position on snacking or grazing. Make snacky carbs available and if possible a Pediasure or other nutrition supplement.
- Side conversation going on in What’s App:
Yaffi: I’m a fan of Orgain for kids when needed.- Diana: Oh me too. I drink it myself most days. I’m on the fence about the grazing situation…I do think that parents need to loosen up about WHAT is available, but I’d also rather not see a kid grazing all day long because that may interrupt the kid’s appetite for the next big meal, which will likely contain a more health-supportive nutrient balance.
- Yaffi: #individualizedcare
- Side conversation going on in What’s App:
- Examine the table dynamic–is there pressure? Parents can focus on providing more suitable food vs pressuring the kid to feed themselves. Remember the one-on-one help I mentioned, yeah that’s this.
- Depending on the age and development of the child, it may be appropriate to have a gentle conversation with the child. Focus on discussing the importance of
- taking care of yourself by getting enough food
- taking time to focus on the meal before moving on to other tasks

More Practical Tips
- Eat smaller meals throughout the day. Be prepared with snacks. Good snacks. Ones you want to eat. Veggies and fruits, crackers and cheese, Oreos, jerky, nuts, granola bars, yogurt, hard-boiled eggs… wait I think I’m menu planning now. Back to the list.
- See if there is a way to increase the nutrition in the food you’re serving. I also love this pdf, ways to increase nutrition provided in food, by Natalia Stasenko, dietitian and founder of the EasyBites App. The standard “add butter and cream to everything” is just unpalatable. And it can disrupt bowel patterns. While butter is important to me, variety is the spice of life. And I like not being constipated. But you know, that’s just me.
- Focus on breakfast. Having breakfast sets the tone for the day. Something. It’s food. Eat the food. This meal, before the meds kick in, is a great time to focus on balance and satiety. If the morning is too hectic, see if you can set something up the night before or eat something convenient–cereal, instant oatmeal, etc.
- Create a meal schedule and stick to it. Yeah, this isn’t really in line with Intuitive Eating (IE). Sometimes the alarm clock can help you meet your body’s needs and that’s ok.
- Liquid nutrition– Orgain, for me. I like the dairy one with 16g protein. Vanilla and chocolate. Smoothies are also great. You can easily and inexpensively boost the protein and calcium in a tasty smoothie by adding ¼ block of tofu. But don’t sneak it in. That won’t end well. We don’t sneak food.
- Consider a multivitamin. Different dietitians have differing opinions on whether a multivitamin is necessary for kids. Speak with your dietitian to determine what’s right for your family.
- Some people may benefit from an appetite stimulant. This is a conversation to have with your provider–the one with the medical chart, remember?
- Make sure to include outside play when possible and safe. Sunlight and smiles.
Sunlight and smiles.
I think I’ll go get some of that right now.
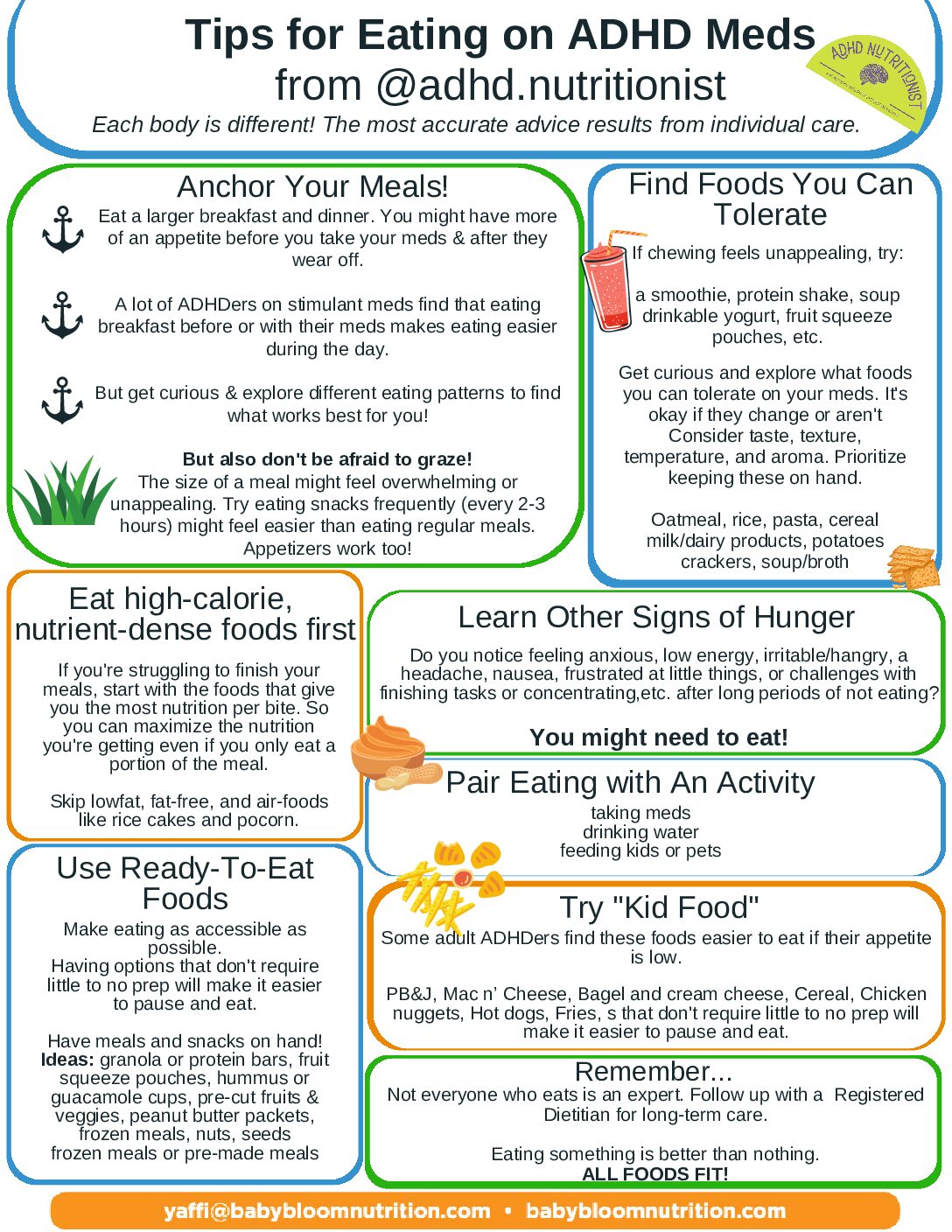
Need something handy?
Here is a great tips sheet full of information from Rebecca King, RD, @adhdnutritionist.
A Post-Script about Gaining Weight
Back to answer a reader question: Are there any kids and tween-friendly books about gaining and maintaining weight.
It’s a great question, and also I’m going to completely side-step it. As someone who is training in eating disorder counseling, I really hesitate to give a book regarding body image to a kid. While practical tips would be helpful, there is a huge risk. Kids don’t have the prefrontal cortex fully developed, meaning that critical thinking skills are still being developed.
I will say that parents can usually safely stay away from most foods advertised to be:
- Sugar-free (that’s just a rabbit hole of its own)
- Low-fat (fat feeds the brain)
- Reduced calorie
- Lean
Giving a child direct access to a resource for manipulating food intake to change body shape carries a much greater risk than reward. Kids are not mature enough to be in charge of their own nutrition. This is why Intuitive Eating isn’t the right way to go with kids–they need the added structure that other Responsive Feeding guidelines provide.
However! However, there are books on having ADHD that could help with validation and other aspects. This can lead to gentle conversations about food and food dynamics in the family. This is a list from ADDitude magazine. I have not read these and can’t vouch, but I’m open to feedback and very happy to adjust the list as I receive it.


Recent Comments